A: There are more than 354 ophthalmic medical disorders.
Here are further guidelines.
What are the skills and knowledge required of an ophthalmologist?
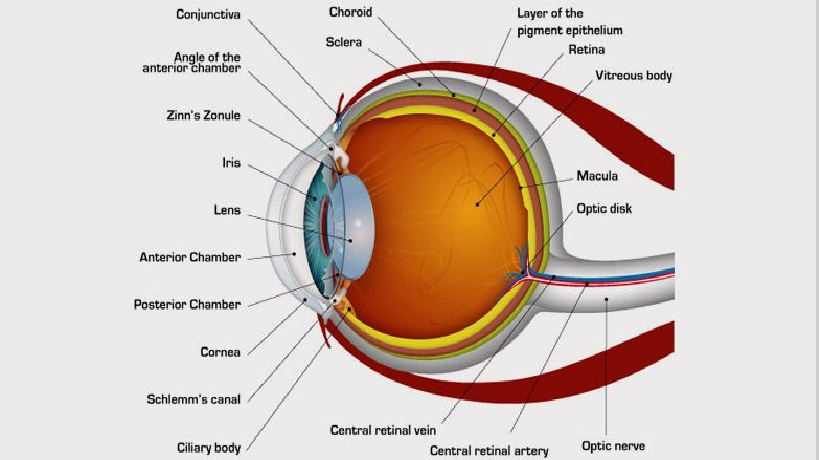
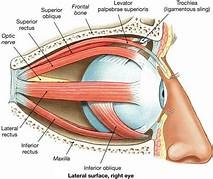
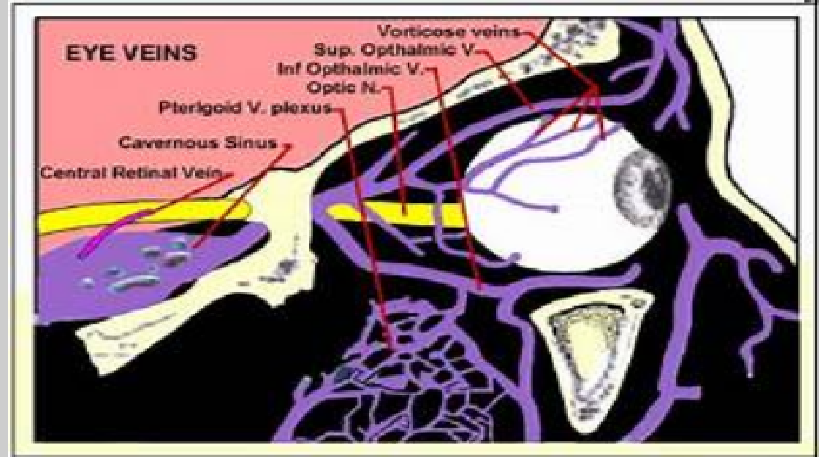
Anatomy, Physiology and Pathology of the Human Eye






|
Eye Emergencies
Eye Emergencies: Types, Symptoms, and Prevention
Ophthalmologist
Sudden Loss of Vision
Sudden Loss of Vision and Slow Loss of Vision
|
Eye Emergency Symptoms
|
What are the causes of sudden painful loss of vision? Sudden painful loss of vision can be due to the following causes: (1) Keratitis (2) Conjunctivitis (3) Scleritis (4) Uveitis (5) Angle closure glaucoma What are the causes of sudden painless loss of vision? Sudden painless loss of vision can be due to the following causes: (1) Retinal vascular occlusion (2) Retinal detachment (3) Optic neuritis (4) Retinoblastoma What are the causes of gradual painful loss of vision? Gradual painful vision loss can be due to the following causes: (1) Keratitis (2) Scleritis (3) Chronic iridocyclitis What are the causes of gradual painless loss of vision? Gradual painless loss of vision can be due to the following causes: (1) Cataract (2) Refractive error (3) Diabetic retinopathy (4) Age-related macular dystrophy/macular degeneration (painless) (5) Retinitis pigmentosa Blindness Blindness: What is it? Being unable to see from both eyes. What is another word or term for being blind? Being completely blind Is there a difference between being blind and being visually impaired? Yes. What is vision loss/visual impairment? Vision loss is a state of impairment to the vision of the eye, which can be complete or partial, permanent or temporary, and unilateral or bilateral. Sudden loss of vision and slow loss of vision: What is the difference? The causes are different. How many causes of sudden loss of vision are there? At least 11. What are the causes of sudden loss of vision? 1. Detachment of the retina 2. Occlusion of the retinal vessel or artery 3. Vitreous hemorrhage 4. Amaurosis fugax 5. Glaucoma 6. Optic neuritis 7. Ocular migraine 8. Drugs 9. Giant cell arteritis 10. Trauma 11. Other conditions Medical history relevant to the issue Have you asked about the proper medical history relevant to this case? What is the medical history relevant to this case? How can visual impairment be described? Complete Partial Permanent Temporary Unilateral Bilateral Sudden Gradual Painful Painless The person can see normally relevant to their age. The person has come in for a routine checkup. How is visual loss classified? Sudden loss of vision Gradual loss of vision Painful loss of vision Painless loss of vision What medical history is necessary for sudden loss of vision? When did it start? Where did it start? How did it start? How long has this been present? Was this sudden or has this progressed? Did the sudden loss of vision occur with pain or without pain? Does the vision loss affect one or both eyes? Is the vision loss total or does it affect only a specific part of the field of vision? Are there other vision symptoms, such as floaters, flashing lights, halos around lights, distorted color vision, jagged or mosaic patterns, and/or eye pain? Are there any risk factors that may cause eye problems? What are the 8-point eye exam findings according to the American Academy of Ophthalmology? 1. Visual acuity 2. Pupils 3. Extraocular motility and alignment 4. Intraocular pressure 5. Confrontation visual fields 6. External examination 7. Slit-lamp examination 8. Fundoscopic examination What is the treatment? Treat the underlying cause. |
| Term | Definition |
| Abrasion | Defect of the corneal epithelium. Stains with fluorescein. Usually heals within 24 – 48 hours |
| Contusion | Result of blunt injury, either at site of impact or distant to it |
| Closed injury | The wall of the globe is intact but structures inside the eye are damaged |
| Rupture | Jagged open injury due to blunt injury, often away from the site of injury at the weakest points of the globe: concentric to the limbus, just behind the insertion of the extraocular muscles or at the equator |
| Open injury | A full thickness break in the wall of the eye; can follow either sharp or severe blunt injury |
| Lamellar laceration | Partial thickness wound caused by a sharp object |
| Laceration | Full thickness penetration |
| Penetration | Entry wound only |
| Perforation | ‘Through and through’ injury; an injury that goes right through the eye, causing both entry and exit wounds |
|
If you have a problem that you feel is an emergency or life threatening, call 911 immediately or go to the nearest emergency room. What are ophthalmological medical emergencies? How should you do a quick assessment, diagnosis, and treatment of a person reported as an ophthalmological medical emergency? * Acute Angle-Closure Glaucoma * Acute Multifocal Placoid Pigment Epitheliopathy * Acute Orbital Compartment Syndrome * Acute Retinal Necrosis * Alacrima * Angle Recession Glaucoma * Aphakic and Pseudophakic Glaucoma * Best Disease * Central Serous Chorioretinopathy * Chalazion in Emergency Medicine * Complications and Management of Glaucoma Filtering * Conductive Keratoplasty Hyperopia and Presbyopia * Congenital Anomalies of the Nasolacrimal Duct * Corneal Laceration * Corneal Ulceration and Ulcerative Keratitis in Emergency Medicine * Dacryoadenitis * Dacryocystitis * Drug-Induced Glaucoma * Dry Eye Syndrome * Eales Disease * Emergency Care of Corneal Abrasion * Emergent Treatment of Acute Conjunctivitis * Endophthalmitis * Exudative Retinal Detachment * Fuchs Heterochromic Uveitis * Glaucoma, Angle Closure, Acute * Glaucoma, Angle Closure, Chronic * Glaucoma, Suspect, Adult * Globe Rupture * Hordeolum and Stye in Emergency Medicine * Hyphema Glaucoma * Intermediate Uveitis * Intraocular Foreign Body * Iris Prolapse * Iritis and Uveitis * Juvenile Glaucoma * Juvenile Idiopathic Arthritis Uveitis * Lacrimal Gland Tumors * LASIK Hyperopia * Lattice Degeneration * Lens-Particle Glaucoma * Low-Tension Glaucoma * Macular Hole * Nonpseudophakic Cystoid Macular Edema * Obstruction Nasolacrimal Duct * Ocular Burns * Ocular Hypotony * Periorbital Infections * Phacolytic Glaucoma * Phacomorphic Glaucoma * Phakic IOL Hyperopia * Pigmentary Glaucoma * Plateau Iris Glaucoma * Posner-Schlossman Syndrome * Postoperative Corneal Edema * Postoperative Endophthalmitis * Primary Congenital Glaucoma * Primary Open-Angle Glaucoma * Proliferative Retinal Detachment * Pseudoexfoliation Glaucoma * Retinal Artery Occlusion * Retinal Detachment * Retinal Vein Occlusion * Rhegmatogenous Retinal Detachment * Secondary Congenital Glaucoma * Sudden Visual Loss * Toxic Anterior Segment Syndrome * Tractional Retinal Detachment * Ultraviolet Keratitis * Unilateral Glaucoma * Uveitic Glaucoma * Uveitis, Anterior, Childhood * Uveitis, Anterior, Granulomatous * Uveitis, Anterior, Nongranulomatous * Vitreous Hemorrhage in Emergency Medicine |
|
Eye Trauma Managing Serious Cases of Ocular Trauma Assessing and managing eye injuries Definitions of terms used to describe eye injuries Eye trauma refers to damage caused by a direct blow to the eye. The trauma may affect not only the eye, but the surrounding area, including adjacent tissue and bone structure. There are many different forms of trauma, varying in severity from minor injury to medical emergencies. Even in cases where trauma seems minor, every eye injury should be given medical attention. What Causes Eye Trauma? When the eye is hit with blunt force, it suddenly compresses and retracts. This can cause blood to collect underneath the hit area, which leads to many of the common symptoms of eye trauma. Symptoms of Eye Trauma Symptoms of eye trauma may include: •Pain •Trouble seeing •Cuts to the eyelid •One eye not moving as well •One eye sticks out •Blood in the clear part of the eye •Unusual pupil size or shape •Something embedded in the eye •Something under the eyelid that cannot be easily removed Treatments for Eye Trauma Every eye injury should be given medical attention; do not touch, rub or try to remove any object in the eye. If the eye has been cut or there is an object in the eye, rest a protective shield – such as a paper cup – on the bone around your eye. Make sure there is no pressure on the eye itself. Seek immediate, professional medical attention. In minor cases of trauma, such as a black eye from a sports injury, applying cold to the affected area can help bring swelling down, and allow the affected area to heal faster. However, even in cases where trauma seems minor, every eye injury should be given medical attention. The best way to avoid eye trauma is to prevent it by using protective eyewear while doing things that may put them at risk. Activities include home repair, yard work, cleaning, cooking, and playing sports. In most cases of injury, people report not properly protecting their eyes – which shows that proper precautions may prevent an eye injury. |
Most common eye conditions
Eye Care
Common, Non-Emergency Eye Problems
|
Are you having any problems with your vision? How long have you had these problems? When do these problems occur? When was your last eye examination? Do you have any family history of eye problems? How is your general health? What medications are you taking? Do you have any allergies? Do you wear glasses/contacts now? Have your glasses/contacts become stronger over the years? Do you work with a computer? Do your eyes ever tire (burn, itch) when reading? Do you ever see double images or halos around images? Do you suffer from eye strain and/or tension headaches? Here are further guidelines. http://www.qureshiuniversity.com/eyecare.html |
|
Ophthalmologist
What is an ophthalmologist? How is an ophthalmologist different from an optometrist and an optician? What is a subspecialist? When should I see an ophthalmologist? What happens during an eye examination? What treatments are available for my eyes? Here are further guidelines. |
|
Q: What should you know and be able to do as an ophthalmologist? What is an ophthalmologist? You are first a physician, than a specialist or super specialist. Ophthalmology is the study of medical conditions relating to the eye. Ophthalmologists are doctors who specialize in the medical and surgical treatment of this organ. A general practice doctor may refer someone to an ophthalmologist if they show symptoms of cataracts, eye infections, optic nerve problems, or other eye conditions. An ophthalmologist is a medical doctor who specializes in diagnosing and treating eye-related conditions. Some ophthalmologists undergo a year or two of fellowship training specializing in one of the many subspecialties of ophthalmology, such as: glaucoma the cornea the retina uveitis refractive surgery pediatrics neuro-ophthalmology plastic and reconstructive surgery ocular oncology Subspecialist ophthalmologists have usually completed training that allows them to work on eye conditions that are complex, involve a specific part of the eye, or affect certain groups of people. They also train more extensively than regular ophthalmologists to perform extremely intricate surgeries on delicate parts of the eye. What conditions do they treat? Ophthalmologists are responsible for the diagnosis, prevention, and treatment of almost all eye conditions and visual issues. However, subspecialist ophthalmologists tend to treat and monitor certain conditions, such as: glaucoma retinal conditions, such as macular degeneration and diabetic retinopathy corneal conditions cataracts cases involving children or childhood eye conditions cases with a neurological cause or component, such as optic nerve problems, abnormal eye movements, double vision, and some kinds of vision loss cases involving complex surgical procedures, such as reconstructive surgery or advanced vision repair Aside from caring for the eyes and vision, an ophthalmologist’s medical training may also equip them to notice symptoms of conditions that do not directly relate to the eye. In such cases, they can refer people for the appropriate treatment. Many ophthalmologists also participate in some form of scientific research focusing on the causes of eye and vision conditions, as well as potential cures. What procedures do they do? Most ophthalmologists are trained and certified to perform a wide range of medical and surgical procedures. The procedures that an ophthalmologist regularly carries out depend on several factors, such as the type of practice and specialty in which they work. Some of the most common everyday procedures that an ophthalmologist will perform include diagnosing and monitoring mild eye and vision conditions. They will also spend time prescribing and fitting glasses and contact lenses to correct vision problems. Subspecialist ophthalmologists tend to perform a smaller range of procedures on a day-to-day basis, focusing instead on the treatment of one condition or a few related conditions. Procedures that subspecialists commonly perform include:
Most people see an ophthalmologist because they are experiencing chronic or severe vision symptoms or signs of eye conditions, such as:
A person may need emergency care from an ophthalmologist if their symptoms include:
A person may also receive a referral to an ophthalmologist if they have conditions or factors that can increase the risk of eye conditions, such as:
A family doctor, pediatrician, emergency room doctor, or optometrist usually refers a person to an ophthalmologist. The American Academy of Ophthalmology recommend that people have a full medical eye exam by the age of 40 years so that an ophthalmologist can create a baseline profile of their eye health. Having an eye health baseline is important because it makes it easier for doctors to spot or track eye or vision changes, which are often subtle and difficult to detect. Even healthy people can suddenly experience severe eye conditions. Vision tests and eye exams are procedures an optometrist may perform.Unlike ophthalmologists, optometrists and opticians are not medical doctors. However, members of all three distinct professions can, and frequently do, work in the same office or practice. Optometrists are healthcare professionals who provide primary vision care. Optometrists hold a Doctor of Optometry (OD) degree, which requires the completion of 3–4 years of college and then 4 years of optometry school. While the procedures that they perform vary between states and individual practices or clinics, most optometrists:
Opticians are a type of healthcare technician. They are specially trained to help design, confirm, select, or fit corrective vision devices, including contact lenses and eyeglass lenses and frames. Opticians cannot diagnose or treat conditions and must follow the prescription and guidance of optometrists and ophthalmologists. The other eye healthcare professionals who frequently work with ophthalmologists and optometrists include:
|
|
Pediatric Ophthalmology Q: How do you diagnose and treat ophthalmic medical conditions in children? Eye Testing for Newborn Eye Testing for Infants Eye Testing for Preschool Children |
| Ophthalmology History |
| What Does 20/20 Vision Mean? |
| Glossary of Ophthalmology Terms |
| Ophthalmology Sections |
| Snellen Eye Test |
| Digital Retinal Photography |
| Corneal Topography |
| Computerized Automated Refractor |
| Automated Non-contact Tonometer |
| Automated Visual Field Perimetry |
| Marco TRS Automated Refraction System |
| Computerized Patient Records System |
Ophthalmic instrument and equipment manufacturers
Who are the quality ophthalmic instrument and equipment manufacturers? What materials do you need to manufacture ophthalmic instruments and equipments? How are ophthalmic instruments and equipments manufactured? Here are further guidelines. |
Refractive errors
Q: What does it mean when someone has 20/20 vision? Q: What are refractive errors? Q: What causes refractive errors? Q: What are the symptoms? Q: What is the difference between reading glasses and distance glasses? Q: How often and how long should plus lenses be used? Q: What if problems such as tired eyes are experienced when using plus lenses? Q: Why do many people need stronger minus glasses year after year? Q: Are plus lenses harmful in any way? Q: How far should the eyes be from the book or computer or other close object when using the reading glasses? Spectacles Fashionable Frames Quality Lenses Q: What are Polarised lenses? Q: What are Transition lenses? Q: What are Polycarbonate lenses? |
| Eye Injuries |
| Low Vision |
| Eye Safety |
| Retinal Detachment |
Cataract
What is the best treatment available for treating cataract? |
Diabetic retinopathy
|
| Health care and desktop computer monitor |
| Laser vision correction surgery |
| Retina and vitreous consultation including evaluation and treatment of age related macular degeneration |
| Cornea transplantation |
| Management and treatment of eyelid and orbital cancers |
| Management and treatment of thyroid eye disease |
| Cosmetic eyelid surgery |
| Reconstructive eyelid and orbital surgery |
| Glaucoma evaluation and treatment |
| Evaluation of all pediatric eye conditions |
| Evaluation of genetic conditions which affect the eye or visual system |
| Eye Health Organizations |
|
People often complain of red eyes, frequent watering, and eye strain. What precautions should people take to avoid it? Computer vision syndrome is getting common these days with the increased use of computers. What is the solution? What are the precautions you would advise for general eye care? What is the difference between an ophthalmologist, an optometrist and an optician? What are the best things about your specialty? What are the worst things about your specialty? Why did you choose your specialty? What types of clinical cases do you commonly see? Briefly describe a typical day. What are the varieties of lifestyles within your field? How do you see your discipline changing over the next decade? |
|
On November 14, 2010, an 18-year-old boy from Baramullah was diagnosed with trauma and retinal detachment at SKIMS. Is that correct? Treatment outside the state was advised. Why does a retinal detachment need treatment outside the state? How many ophthalmologists are there in the state? Why didn't the state department of health impart training to existing medical doctors or ophthalmologists to treat such cases within the state? |
| Eye Disability |
|
There is no exact verified number of blind people in the state. There is no exact verified number of people with eye disabilities in the state. A Community Ophthalmology Unit is opened at a primary health center. How did they determine that a Community Ophthalmology Unit at a primary health center at specific location is required? Who has the duty to maintain an exact verified number of blind people and those with eye disabilities in the state? Who has the duty to research and treat these cases? How many people in your state are completely blind? What is the cause of blindness? What is their profile? Where is the exact lesion? Is their a hope for them to regain their vision? What have you done? How can I/we help? Are you as an ophthalmologist facing a most difficult case? If yes, feel free to communicate and consult. admin@qureshiuniversity.com |
Ophthalmic instrument and equipment manufacturers
Gallery of Eye Examination Equipment.
Eye Diseases and Disorders
Research documentation
Consultation documentation
|
How should an ophthalmologist record consultation documentation? Record the exact reasons for consultation, including the exact statement or question relevant to the consultation. At this point, what are the reasons for the consultation? Date: August 2, 2022 Time: 1:30 PM Location: 836 West Wellington Suite 5 Ophthalmology 773-975-1600. Ophthalmology (773) 296-3937 Name of the ophthalmologist: Kelley Bohm, MD, Illinois Masonic Medical Center 836 W. Wellington Ave., Chicago, IL 773-296-8000 Fax: 7732967787 https://chicagoeyeinstitute.com/. Reasons for consultation: 1. Routine checkup. 2. Issue that needs research and deliberations with current ophthalmologist. I have faced the bright light of the computer screen while researching for 8 hours per day, 56 hours per week, over the last 22 years, 1999-2022, in Chicago, Illinois, United States. The results of my research are displayed at www.qureshiuniversity.com/university.html. The current ophthalmologist who will see me on August 2, 2022, at 1:30 PM needs to do some research on this issue. What can be the effects of using a bright light while researching 56 hours per week for 22 years? I can focus on the computer easily. If immediately, I need to see 12-point size font at room light brightness or font that is increased to 14- or 16-point size for luminous intensity. I would prefer if you research some eye dark room exercises for me that will counter the brightness of computers. What did you understand? What do you suggest? I can guide 72 types of physicians, including ophthalmologists. Take a look at this: www.qureshiuniversity.com/physicians.html Take a look at this: https://qureshiuniversity.com/ophthalmologyworld.html What are the concerns relevant to this issue? A person says one thing. The ophthalmologist writes something else. See the examples. Why is there a need to elaborate on this issue? On July 19, 2022, I talked to one of your representatives. This was after I received your phone call. I need to arrange an appointment. I was surprised when your representative told me that previously, on October 30, 2019, at 1 PM, I had come for blurred vision and/or cataracts. This is not true. Previously I had come for a routine check-up. Someone else recommended a routine check-up and to get my routine eye pressure checked. That was normal. Your previous doctor lied. I did not ask for a consultation for blurred vision and/or cataracts. I need to have confidence in the ophthalmologist I will be seeing. I would appreciate if this document is provided to the ophthalmologist I will be seeing before our in-person consultation. Administrative skills: What are various examples? Accuracy There are many more. You will have to do lots of research and come up with answers to these research questions. An email communication is required compared to an in-person meeting. I will come for the scheduled meeting but an email is also required to provide answers to these questions. All ophthalmologist needs to research this topic. What is the topic? Bright light from the computer and its effects on eyes How does the bright light from the computer affect the eyes and eyesight? To answer this question, we have to elaborate on many questions. Bright light from the computer and effects on the eyes: What happens? Take a look at this. What happens to the iris in dim light? In dim light, the iris causes your pupil to expand, allowing as much light as possible into your eye. What will happen to the iris in bright light? In bright light, the iris causes the pupil to contract so that less light can enter. Questions you need to answer. What will happen if you move from a bright light area to a dim light area? What will happen to the iris in reaction to the bright light from the computer for 8 hours per day, 56 hours per week for 22 years, 1999-2022? What advice do you have for this situation? |
Teaching skills relevant to this profession, preferably via the Internet.
|
What are various emergency ophthalmology symptoms? Answer What are various emergency ophthalmologist diagnoses? Answer |
Last Updated: July 30, 2022